Scourge of drug abuse threatens HIV gains
Sunday Mail Zimbabwe
Zimbabwe has made commendable strides in fighting HIV and Aids in recent years, with the latest milestone being surpassing the 95-95-95 United Nations Programme on HIV and Aids (UNAIDS) targets ahead of time.
The goals are to ensure that 95 percent of all people living with HIV know their status, 95 percent of all people diagnosed with HIV receive sustained anti-retroviral therapy (ART), and 95 percent of all people receiving ART have viral suppression by 2025.
However, a new threat that might potentially scupper these huge gains is emerging.
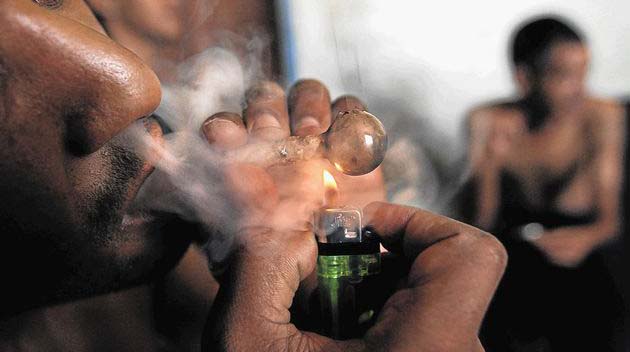
A recent year-long situational analysis of injection drug use (IDU) in five provinces, which was meant to inform HIV and TB programming on people who use and inject drugs, revealed that rising substance abuse has the potential of creating a wave of new HIV infections.
The National Aids Council (NAC), the Zimbabwe Civil Liberties and Drug Network (ZCLDN) and the Ministry of Health and Child Care (MoHCC) spearheaded the research, which revealed widespread IDU and sharing of injection materials.
The study, whose results were released on November 18, indicated that anti-retroviral medicines designed to fight HIV are being used as an ingredient to produce highly addictive drugs.
Young people were reportedly swallowing, snorting and injecting dangerous substances laced with psychiatric medications such as diazepam into their bodies and potentially exposing themselves to HIV and Aids.
“Bluetoothing”
Furthermore, the study found unsafe injecting practices such as inoculating the wrist, thigh, groin or neck, with reports of abscess caused by injection.
One of the most shocking forms of drug abuse, according to the findings, is that youths are exchanging blood — a practice they call “bluetoothing”.
This is done to cut the costs of the drug, as a user can draw blood from one intoxicated user to inject it into the next person to “get high”.
“Many key informants mentioned ‘bluetoothing’, a practice whereby blood is taken from someone who has just injected and then injected in another person in the hope they will receive a small amount of the substance the other person just injected,” reads the report.
“Focus group discussions’ participants confirmed that sharing injection equipment is common, even though the risks to HIV transmission are known. Respondents said syringes and needles are often shared between two to four people. The decision whether or not to share equipment mostly depends on family or friendship bonds or on physical appearance (“if you don’t look fit, you find your own syringe”).
“Respondents explained methods to reduce risks of sharing such as waiting eight minutes to use a syringe that has already been used by someone else, or burning a used needle with a lighter to sterilise it,” it added.
Over one-third of the survey sample said they had shared injections and more than a quarter had done so in the past month.
More than half of the women interviewed reported having been injected.
Most commonly used substances by research participants were cannabis (known as skunk), alcohol and cough syrup (codeine).
Medical and Dental Private Practitioners of Zimbabwe Association president Dr Johannes Marisa said IDU can be a direct route of HIV transmission if people share needles, syringes or other injection materials that are contaminated with the virus.
“Similarly, drinking alcohol and ingesting, smoking or inhaling drugs are also associated with an increased risk of HIV.
“These substances alter judgment, which can lead to risky sexual behaviours like having sex without a condom and having multiple partners that can make people more likely to get and transmit HIV,” he said.
“In people living with HIV, substance use can hasten disease progression, affect adherence to antiretroviral therapy (HIV medicine) and worsen the overall consequences of HIV.”
NAC chief executive officer Dr Bernard Madzima said the parastatal had commissioned the research to ensure the country attains the global goal of ending Aids by 2030.
“NAC, in partnership with MoHCC and the ZCLDN, with financial support from the Global Fund and UNAIDS, commissioned a situational analysis of drug use and injection in Harare, Bulawayo, Mashonaland Central, Mashonaland West and Manicaland provinces.
“We believe such research will help us against new threats that we face in the battle against HIV.” It is anticipated that these findings and recommendations
will provide valuable information to enable programming for people who use and inject drugs, as well as giving guidance for legal reforms.
There is also concern that young people involved in substance and drug abuse are developing mental health challenges, leading to high risk of HIV infection.
Research done by the Health Professionals Empowerment Trust in Zimbabwe showed that 50 percent of admissions to mental institutions have been attributed to substance-induced disorders.
On Thursday, Zimbabwe joined the rest of the world in commemorating World Aids Day, as new interventions continue to be enforced to fight HIV and Aids.




